The COVID-19 pandemic has created an unprecedented situation worldwide, causing millions of deaths and significant damage to the world economy. For more than a year, people have heard and hoped for herd immunity that may be achievable in the long-term with near-universal vaccination. Do the low infection rates around the world suggest that COVID-19 herd immunity is just around the corner?
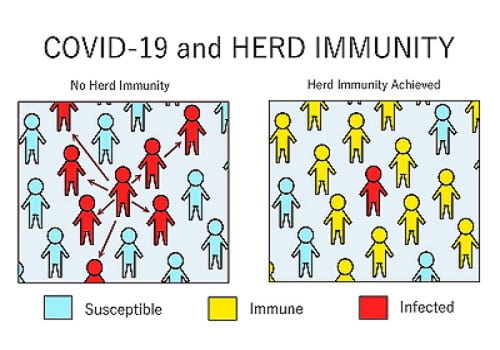
It’s been more than a year since the world first encountered the highly contagious SARS-CoV-2 virus. The resilient coronavirus has managed to proliferate and spread across communities despite social distancing measures and other precautions to stop transmission. Now that multiple COVID-19 vaccines have been authorized and rolled out for use, people are positive about developing “herd immunity”. According to the United States Centers for Disease Control and Prevention, herd immunity refers to the sufficient proportion of the population that become immune to a particular disease due to the development of antibodies either from vaccination, or previously contracting the disease.
If majority of the population becomes immune after vaccination, they would not be able to spread the infection further to vulnerable population. Thus, herd immunity ensures the protection of the remaining population and reduces the risks of transmission. Developing herd immunity seems like a practical solution for a fight against COVID-19 infection and therefore vaccine inoculation drives are at full swing. There isn’t any “magic threshold” but, usually 50-90% population needs immunity before the infection rates start to decline, however the number can vary depending on how contagious the virus is. For COVID-19, the herd immunity is estimated to be between 70-90%, given that the immunity lasts longer.
How Can We Achieve Herd Immunity with SARS-CoV-2?
While wearing masks in public, social distancing, and reducing the level of interaction can help to slow down the infection rates, the virus might mutate as communities open up broadly and become even more contagious. However, there are two ways to achieve herd immunity, either the large proportion of the population gets vaccinated or infected with the virus. Achieving herd immunity in the United States would require more than 230 million Americans to get infected. However, this could lead to more hospitalization, ICU admissions, and cost millions of lives. The patients who suffer from mild infection might also have severe illness for weeks or other long-term side-effects. Therefore, achieving herd immunity through infection becomes painfully ill-conceived thought.
Another way to achieve a herd-immunity threshold is through high vaccination rates, immunizing mass population so that the society could return to normalcy. Vaccine inoculation to 70-80% of the population for COVID-19 virus will not only protect the vulnerable populations at high risks but also extend the immunization benefits beyond the directly targeted population. Some of the vulnerable groups that depend on herd immunity for achieving protection against the diseases include:
• People with compromised immune functioning
• People on chemotherapy treatments
• People suffering from HIV
• New-borns and infants
• Elderly people
Why is Vaccine Equity Essential to Develop Herd Immunity?
While more than 1.65 billion doses of vaccines have been administered in rich nations, only 0.8% of all vaccines have been allocated to poor countries. Wealthy nations have focused more on securing vaccines for their populations while ignoring to make investments in cooperative initiatives for fair distribution of vaccines across the globe. However, the global coverage of vaccines is imperative to manage the transmission of COVID-19. The imbalance is creating a need to move past beyond outdated charitable models and instead focus on amplifying the manufacturing and distribution capacity throughout the world in order to increase immunization. The international community need to empower nations by technology transfer or passing intellectual property waivers in the World Trade Organization for vaccines so that poor countries can produce their own vaccines.
Vaccine nationalism may not be the best solution to defeat the spread of virus. As wealthy countries are rolling out domestic vaccination plan, the new and emerging variants are reducing the effectiveness of vaccines against the virus. Even with vaccination shields, the rich countries are vulnerable, and their economies are also at risk. The International Chamber of Commerce predicts that if poor countries are not immunized, the global economy may lose across USD9.2 trillion whereas funding for the Access to COVID-19 Tools (ACT) would require only USD22.9 billion. Besides, global allocation might postpone the domestic vaccine roll-out but doing so will contribute to global herd immunity.
Obstacles for Achieving Herd Immunity
• Vaccine Hesitancy
Some people are reluctant to get vaccinated due to lack of information about the safety of vaccines, or widespread misinformation about them. Besides, religion, political party affiliation, or ethical obligations are adding to vaccine hesitancy. According to a study, one in four young adults do not want to get vaccinated, jeopardizing the health of older unvaccinated adults and facilitating the rise of vaccine variants. However, education and public health messaging can encourage youth and young adults to reduce vaccine hesitancy.
• Emergence of New Variants
As long as there are unvaccinated populations across the world, the COVID-19 virus will continue to mutate and become more dangerous. Even if the wealthy nations successfully achieve herd immunity, the risk of transmission would not reduce, and the booster shots might be required to ensure protection against the variants that could evade the immune response provoked by current vaccines. Besides, the emergence of new strains across the world due to mutation in the spike protein of the coronavirus may not induce antibody response in the infected person.
• Delayed Arrival of Vaccinations for Children
Children have been less susceptible to the coronavirus but not all have escaped unscathed. Besides, infected youngsters have unintentionally passed the illness to others, and thereby increasing the overall infection rates. Although many vaccines are under trial to determine their efficacy against the coronavirus for children, it is only a matter of time when the virus mutates and start attacking the young population. Brazil’s devastating wave of coronavirus is targeting younger age groups and pregnant women. Despite the growing paranoia, many young mothers are not willing to seek vaccination for their children due to misinformation about vaccines and their potential side effects.
• Limited Evidence on Immunity Post-COVID Infection
Some studies suggest that infection with SARS-CoV-2 offers protection against the virus for at least a year. As the antibodies enhance immune response and confer strong resistance against variants of coronavirus, getting infected guarantees some level of protection. The level of immunity that vaccines offer varies depending upon how one’s body responds to it. A single dosage provides some level of protection, but second dosage is essential to achieve full immunity. While scientists have evaluated the efficacy of vaccines for most people in the first few months, they do not have data on the long-term immunity since many vaccines haven’t even completed a year of follow-up.
Conclusion
Vaccinating as many people as possible can be significant in slowing down the spread of the COVID-19. However, achieving herd immunity would not guarantee complete eradication of the coronavirus as it is highly infectious and continues to evolve. Herd immunities vary at global, national, and community level, and change over time, therefore even when the threshold is attained, there would be small outbreaks due to uneven vaccine coverage.
According to TechSci Research report on “Global Coronavirus Vaccine Market By Infection Type (SARS-CoV-2, SARS-CoV, MERS-CoV), By Vaccine Type (Virus Vaccine, Viral Vector Vaccine, Nucleic Acid Vaccine, Protein Based Vaccine and Others), By Product Type (Monovalent Vaccine v/s Multivariant Vaccine), By Route of Administration (Intramuscular, Oral, Intranasal), By Patient Type (Adults v/s Pediatric), By End User (Hospitals, Clinics, Research Institutes, Others), By Region, Competition Forecast & Opportunities, 2026″, the global coronavirus vaccine market is anticipated to grow at a formidable CAGR during the forecast period owing to factors such as the rising incidences of coronavirus infection as well as introduction of new vaccines in the market.
According to another TechSci Research report on “Global Coronavirus Diagnostics Market By Type of Test (Molecular v/s Serology), By User (Multiple v/s Single), By Full Test Time (1 Hour – 12 Hours, Less Than 60 Minutes, 13 Hours – 24 Hours, More Than 1 Day), By End User (Hospitals, Public Health Labs, Private or Commercial Labs, Physician Labs, Others), By Region, Competition Forecast & Opportunities, 2026″, the global coronavirus diagnostics market is projected to reach a market value of USD15.57 billion by 2026. The growth can be attributed to the increasing incidences of coronavirus cases and rising use of diagnostic testing kits for the same.
